Gum disease
Most adults will have gum disease to some degree at least one point in their lives. Superficial inflammation of the gums, known as gingivitis, is the most common form of gum disease. It may result in reddened, swollen or bleeding gums. If this is left untreated it can lead to more serious gum disease irreversibly affecting the underlying bone, known as periodontitis. Untreated periodontitis can lead to loosened teeth, sensitivity, receding gums and eventual tooth loss. Severe periodontitis affects around 10% of the population.
Stages of gum disease
A periodontal probe is used to assess the health of your gums. One way of detecting gum disease is measuring the depth of “pockets” between the tooth and gum. In gum disease these pockets increase in depth. The pockets are also assessed for any bleeding.
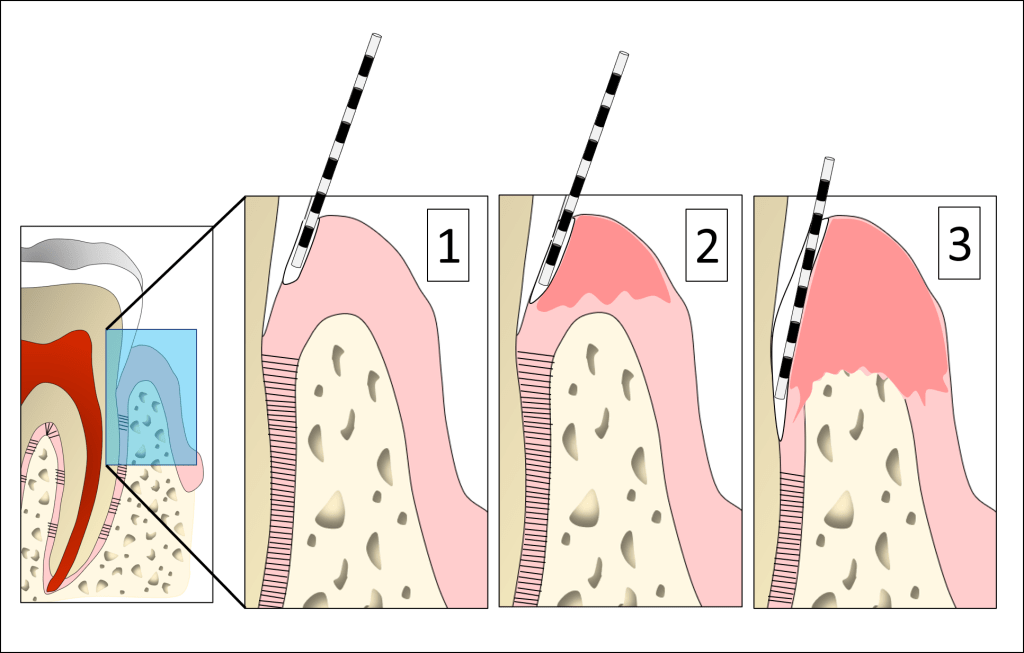
- In health there is a shallow pocket around the teeth between 1-3mm in depth. There is no inflammation or bleeding of the gums during brushing.
- In gingivitis (early gum disease), the gum becomes inflamed and may bleed more. There may be a slight increase in the pocket depths. However, there is no bone loss at this stage.
- In periodontitis (advanced gum disease), there is greater inflammation and increased pocket depths. The underlying bone is lost as gum disease progresses which ultimately can result in mobility and tooth loss.
Causes of gum disease
Dental plaque
Gum disease is primarily caused by bacterial plaque on the teeth. When oral hygiene is inadequate more harmful bacteria build up and cause inflammation within the gums. In some forms of aggressive gum disease very small amounts of plaque can provoke this inflammation. This inflammation over time can lead to loss of attachment of the gum and the underlying bone which supports the tooth.

Smoking
Smoking reduces the resistance of the gums to harmful bacteria. Smokers have more gum problems and lose more teeth than ex-smokers or non-smokers. Even with very good oral hygiene, smokers experience more bone loss and are at greater risk of tooth loss. Smokers do not respond to gum treatment as well as non-smokers. In ex-smokers, the condition of the gums can be improved after just a few years and former smokers respond to treatment better than patients who still smoke.
Systemic disease
Periodontitis and diabetes have a two-way relationship on one another. Diabetics whose blood sugar is not managed have a higher risk of developing periodontitis and conversely, patients with periodontitis have a higher risk of diabetes. On the other hand, diabetics with well managed blood sugar levels do not have a higher risk for periodontitis. Interestingly, the treatment of one disease has a positive effect on the treatment of the other. If you are diabetic it is important to have regular check-ups at your dentist and treat any signs of periodontitis. Equally if you have periodontitis a blood test to check for diabetes may be indicated
Genetic factors
Your genetics play an important role in your susceptibility to periodontal disease. While it is not possible to alter this, it can be helpful to understand why you can have severe disease after making significant efforts with your oral hygiene and dental attendance. The immune system can vary in its response to harmful bacteria. As a result, the condition can be different from person to person. In patients with aggressive types of disease they can react more unfavourably to even the smallest amount of plaque on their teeth. That is why if you are at particular risk of disease your oral hygiene practice may need to be more thorough to control gum disease. We may ask about your close family’s experience of gum disease to understand your individual risk of gum disease.
Medications
Some medications may cause your gums to become overgrown. These include some drugs for epilepsy, angina, high blood pressure and immunosuppressants. This overgrowth can usually be avoided by excellent oral hygiene and, if necessary, altering the medication. Occasionally, we may suggest surgery to reduce the overgrown gums.
Other factors
We know that there are links with stress in relation to periodontitis. While there is more to be understood about this relationship it may play an important role in managing periodontal disease. Other factors that may contribute to periodontal disease include your diet.
Consequences of gum disease
Gum disease often does not cause pain and you can be unaware of active disease for many years. You may notice the following:
- Gums that bleed easily i.e. during brushing (less so in smokers)
- Red, swollen gums
- Gums that feel tender when touched
- Bad breath
- Pus between your teeth and gums
- Sensitive teeth
- Loose teeth
- Gum recession (the teeth may appear longer)
- New spaces appearing between your teeth
- Teeth moving position in the mouth
A reliable diagnosis can only be made by a dentist. Your dentist will probe around the gums to check for bleeding and pockets. They may take X-rays (radiographs) to look for bone loss around the teeth. If you have severe gum disease you may benefit from an assessment with a specialist periodontist.
